Joints – a highly complex matter
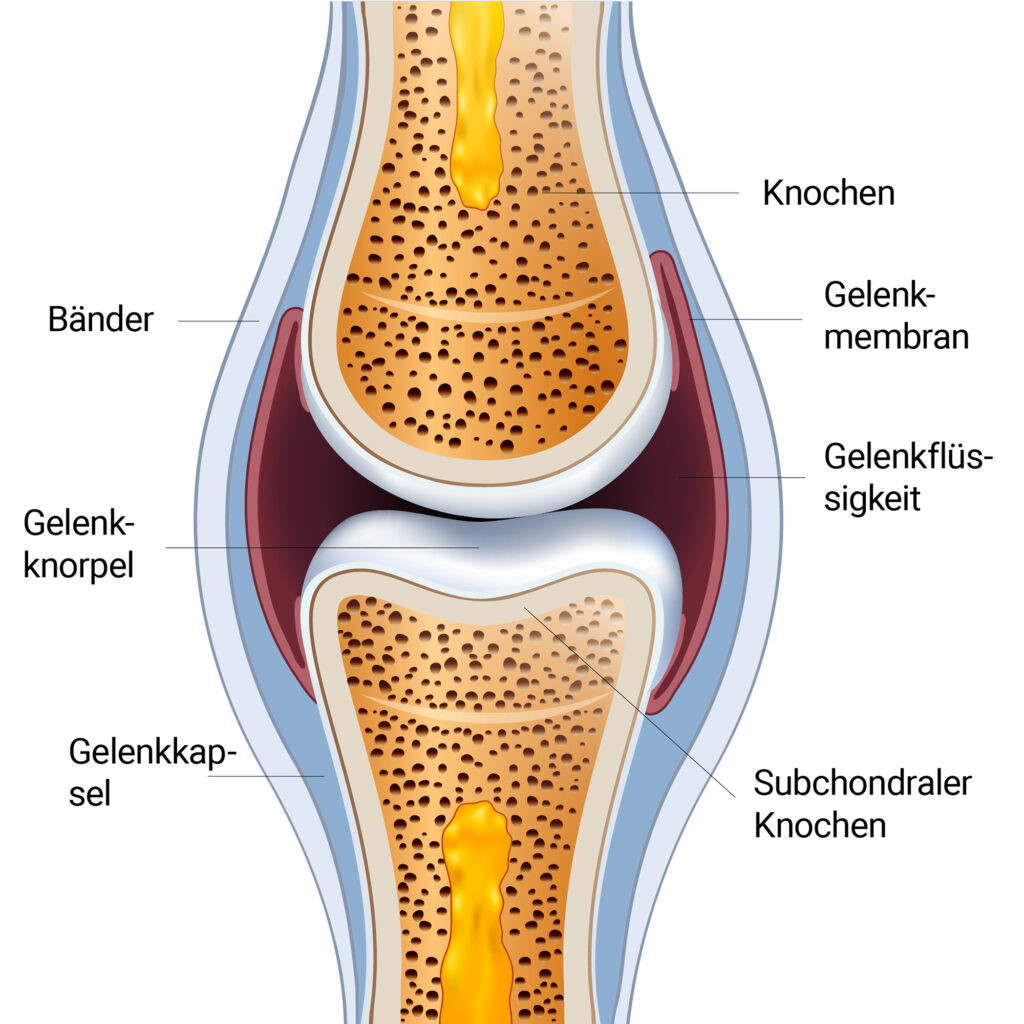
Joint function depends on the integrity of the normal anatomy and proper cellular function of all structures involved in the joint. The following structures belong to a joint:
- Bones,
- Articular cartilage,
- synovial fluid,
- articular membrane,
- joint capsule and
- Band structures.
On both sides of a joint, the bone is covered by articular cartilage, which provides the almost frictionless contact surfaces of the joint. The synovial membrane (inner lining) and the joint capsule (outer part) surround the cartilage and adhere to the bone on both sides of the joint, providing stability and a cavity for the synovial fluid. A joint is further stabilized by the surrounding ligament and muscle structures .
The health of a joint depends on all these structures. All these structures must be functional.
A healthy joint offers a smooth system that is far superior to modern technology. When a disease occurs, it is usually due to a dysfunction of one or more components of the joint.
Only those who know the structure of cartilage can help it:
Articular cartilage is the central structure that forms the joint surface and ultimately its function. In conjunction with the synovial fluid, the articular cartilage is enabled to move the joint almost without friction.
Cartilage is a unique tissue. It has neither blood vessels nor nerve tissue, which dictates its dependence on diffusion for nutrient supply and waste removal.
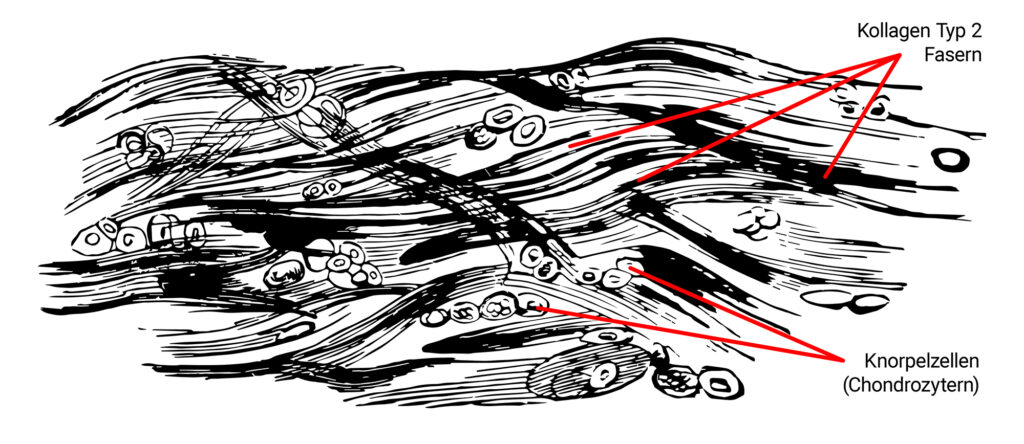
Collagen is the main component of articular cartilage and forms a scaffold for all other cells of the articular cartilage.
Collagen is also the component attributed to the counteraction of tensile stresses on the joint surface.
The primary collagen of articular cartilage is type II and is produced by the cartilage cells. Collagen type 2 accounts for 90% to 95% of the total collagen content in the joint.
It all depends on the mechanism:
Osteoarthropathy is a general term defined as any disease of the joints and bones. It is derived from the Greek words osteo (bone) and arthron (joint).
A more specific term that refers to a disease of the articular cartilage is osteoarthritis, defined as a disorder of the movable joints characterized by degeneration and loss of articular cartilage
The tissues of the joint have a certain capacity for repair. However, some tissues such as bone are very adept at repair, while others such as articular cartilage are less adept. Osteoarthritis has thus been defined as the point at which the restorative repair processes are overwhelmed by the degradative processes.
Degeneration of articular cartilage occurs with the loss of aggrecan and type II collagen. The body’s own cartilage-degrading protein (MMP) plays a decisive role in osteoarthritis. Interleukin 10 and TNF-ß are its natural antagonists, which restore the balance in the joint.
Recognize osteoarthritis at an early stage:
A filled joint (synovial effusion) is a common finding, especially in joints with excessive joint stretching. Synovial effusion is thought to be triggered by inflammatory events in the joint and is partly due to increased vascular permeability (ingress) and a decrease in lymphatic drainage (egress). This increase in fluid leads to abnormal use of the joint for both mechanical and pain-related reasons.
If the inflammatory process is not controlled, it can lead to changes in the joint capsule, which is often observed as a restricted range of motion.
As the disease progresses, pain and further movement restrictions occur.
Cartilage repair
The modulatory or regulatory cytokines such as Il-4, Il-10 and Il-13 have effects that balance or modulate the pro-inflammatory cytokines, namely Il-1 and TNF-α. It has been shown that they inhibit the synthesis of Il-1 and promote the synthesis of natural inhibitors, in particular tIMPs and Il-1Ra.
An observation made in 1743 that “cartilage, once destroyed, never heals” is still true today.
Modern nomenclature defines healing as the restoration of structural and functional integrity, while regeneration indicates that the tissue will be identical to the original.
Repairs, on the other hand, have a limited meaning and suggest that cells and tissue structures replace the damaged tissue, but the tissue does not necessarily return to its original structure or function.